Overcoming these challenges and planning for a successful future comes down to a strategic approach to patient care and operational management. Our recent study, in partnership with MGMA, dives into addressing these challenges facing facilities across the nation — and providing four specific strategies to employ as you begin planning for 2025 and beyond.
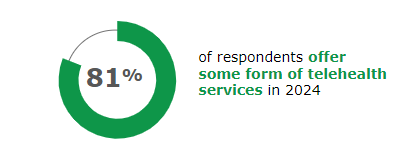
1. Leverage telehealth
81% of healthcare leaders report offering some form of telehealth services in 2024 — and with patient demand for shorter wait times and increased access to care, expanding technology services is going to be essential in the years ahead. 43% of practices report that telehealth had a positive impact on patient wait times.
With the ability to evaluate and treat through tele-services, facilities can create efficiencies in their operations, by seeing more patients and reducing wait times. Telehealth not only offers effective solutions to patients who aren’t able to physically visit an office, but also provides flexibility and balance for clinicians. The compounding issues of increased rate of physician burnout and the physician shortage, telehealth is an invaluable asset to alleviate this added challenge. As you plan ahead for the future, look at your telehealth offerings and consider where you may be able to build, expand or offer hybrid services.
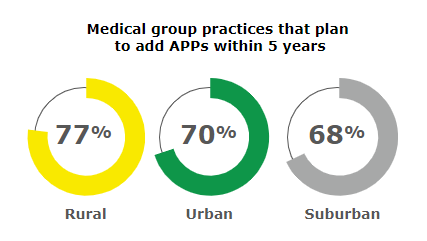
2. Optimize APPs
APPs are a critical link in the chain of healthcare providers as we move into the future. This sector continues to expand with significant expected growth in APP recruitment and staffing. Across all healthcare specialties, APP use and reliance has expanded, with 63% of medical groups reporting plans to add APP roles in 2024, particularly physician associates (PAs) and nurse practitioners (NPs).
With more than seven in 10 healthcare leaders anticipating adding new APP roles in the next five years, APPs are poised to offer operational improvements to your facility, such as extending clinic hours or weekend coverage. In addition, by allowing APPs to independently manage less complex cases, handle routine and non-urgent visits, they offer an effective solution to help combat physician burnout.
Now is a good time to establish how you’ll leverage APPs in your care models — and where you might create opportunities for them to succeed. Federal labor data suggests a 38% growth rate in CRNA, CNM and NP employment by 2032. Therefore, with effective planning today on how to optimize APPs in the coming year, you position yourself as a thought leader at the head of the pack.
3. Focus on Retention
While salaries and signing bonuses certainly grab the attention of many clinicians, the culture of a facility is what truly keeps them. Facilities that focus on creating and building a brand for their organization are likely to see higher retention. Building an atmosphere where clinicians feel like valued partners is critical. Emphasize factors like clinician and license safety, clinical and administrative support systems, and opportunities to advance skills in technology, procedures and devices. These factors are highly valued among clinicians and demonstrate the commitment to career growth and satisfaction.
By focusing on onboarding, day one experience, continued training and open communication, you’ll set the standards for higher clinician satisfaction and lower turnover.
4. Win at recruitment
All of these previously mentioned strategies contribute to effective recruitment. In today’s healthcare market, recruitment goes beyond simply filling gaps in schedules. With 70% of healthcare leaders reporting their organizations need to explore new physician recruitment options, a strong retention strategy is essential. To be strong industry leaders, healthcare facilities must adopt a comprehensive approach to staffing, including establishing physician float pools, leveraging APPs, incorporating tele-hybrid models, and using predictive analytics. With a consultative approach that focuses on connecting to both staff and patients, facilities can strategically manage their workforce and increase overall access to care.
To get more information about the challenges facing healthcare facilities across the country—and dive deeper into the strategies to tackle them—download the full report here.

About the author
Miechia A. Esco
Dr. Miechia Esco is a vascular surgeon focused on full-time locum tenens work and licensed in 15 states. For the past several years she has served as a consultative member on the LocumTenens.com Customer Advisory Board and now serves as the company’s Chief Medical Resource Advisor.





